2020 Project: Bioengineering Approaches to Diabetes Treatment
Note: CATALYST Academy was cancelled in 2020
Faculty Director: Dr. Shivaun Archer, John and Janet Swanson Senior Lecturer
Department: Meinig School of Biomedical Engineering, Cornell University
 Dr. Shivaun Archer is a Senior Lecturer in the Biomedical Engineering Department at Cornell University where she designs, implements, and supervises undergraduate instructional labs for six biomedical engineering courses. Before coming to Cornell, she worked at a small research company specializing in biotechnology, biomaterials, chemical and biological sensors, medical biotechnology, and environmental remediation. Her research interests include nanobiotechnology and tissue engineering.
Dr. Shivaun Archer is a Senior Lecturer in the Biomedical Engineering Department at Cornell University where she designs, implements, and supervises undergraduate instructional labs for six biomedical engineering courses. Before coming to Cornell, she worked at a small research company specializing in biotechnology, biomaterials, chemical and biological sensors, medical biotechnology, and environmental remediation. Her research interests include nanobiotechnology and tissue engineering.
Diabetes is a disorder characterized by hyperglycemia or elevated blood glucose it is the most common endocrine disorder. Thirty million Americans have diabetes, yet many are not aware of it. Diabetics must adjust their intake of carbohydrates and their dose of insulin, in order to maintain blood glucose levels that are near normal. Diabetes has potential long-term complications that can affect the kidneys, eyes, heart, blood vessels, and nerves. These complications appear to be related to the degree of control that the diabetic can maintain over their glucose level. There are two types of diabetes, Type 1 and Type 2. Type 1 diabetics do not produce insulin due to an autoimmune response which attacks insulin-producing pancreatic cells. People with Type 2 diabetes can still make insulin however, their cells have some degree of insulin resistance i.e. the muscle, fat, and liver cells do not respond to insulin signals to remove glucose. This results in a build-up of glucose.
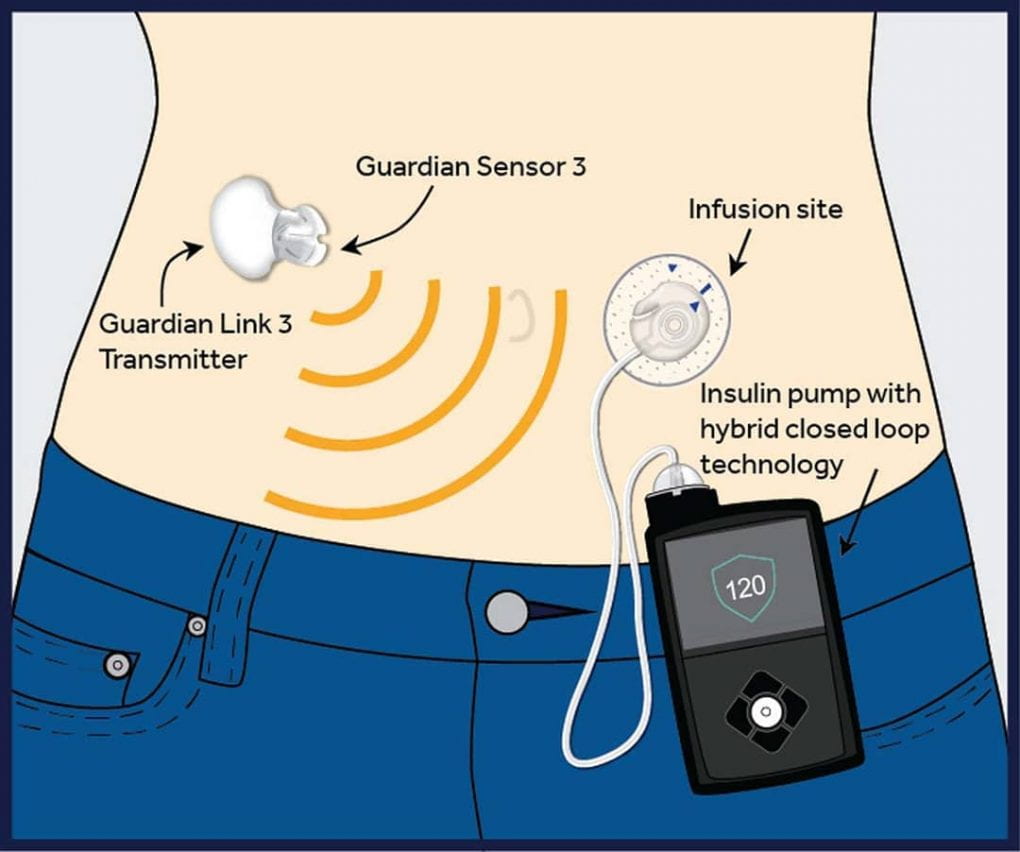 Initial therapy for Type 2 diabetics with mild disease is lifestyle modification: a healthy diet with exercise to help lose weight. If this fails, medication is recommended that increases the number of insulin receptors present on cells, so they become more sensitive to insulin. The only effective treatment in Type 1 diabetes is administering insulin as these patients no longer produce it. There are many different types of insulin and different regimens, but many patients will use long-acting insulin at night supplemented by short-acting insulin before mealtimes. Newer treatment regimens include the use of an insulin pump where blood glucose levels are entered into a machine which then uses an algorithm to pump insulin into the body. In 2016 the FDA approved the first insulin pumps that mimic the way the human pancreas works by delivering small doses of short-acting insulin continuously. The device also can deliver variable amounts of insulin when a meal is eaten. This has been a huge advancement in diabetic care.
Initial therapy for Type 2 diabetics with mild disease is lifestyle modification: a healthy diet with exercise to help lose weight. If this fails, medication is recommended that increases the number of insulin receptors present on cells, so they become more sensitive to insulin. The only effective treatment in Type 1 diabetes is administering insulin as these patients no longer produce it. There are many different types of insulin and different regimens, but many patients will use long-acting insulin at night supplemented by short-acting insulin before mealtimes. Newer treatment regimens include the use of an insulin pump where blood glucose levels are entered into a machine which then uses an algorithm to pump insulin into the body. In 2016 the FDA approved the first insulin pumps that mimic the way the human pancreas works by delivering small doses of short-acting insulin continuously. The device also can deliver variable amounts of insulin when a meal is eaten. This has been a huge advancement in diabetic care.
Other novel treatments being investigated are a combination of tissue engineering and biomaterial approaches to produce functioning pancreatic cells e.g. using stem cells that can act as a bioartificial pancreas. A bioartificial pancreas is a device that can be implanted into the patient and take over the function of insulin/glucose regulation, it contains synthetic materials and functional islet cells encapsulated within a semipermeable membrane to protect them from immunological rejection. The encapsulated islets can act as immune barriers while permitting mass transfer of nutrients, glucose, and insulin to and from the islets.
In the week-long CATALYST project, students will learn about various bioengineering approaches to diabetes treatment. There will be five lab sessions where students will build a simplified model of an artificial insulin pump and investigate the challenges of getting such a device to work using an engineering design approach. In addition, students will learn the basic principles of tissue engineering and will grow pancreatic cells and encapsulate them in alginate. They will test their viability and the ability of the encapsulated cells to produce insulin.

